Express Scripts Weight-Loss Drug Coverage Checker
Coverage Information
When you’re scrolling through your pharmacy portal and see a long list of weight‑loss options, the first question that pops up is usually, “Will my insurance actually pay for this?” If you’re a member of Express Scripts, the nation’s largest pharmacy benefit manager, the answer depends on the drug’s status on their formulary.
What "approved" really means in the Express Scripts world
Express Scripts doesn’t approve drugs in the same way the FDA does. Instead, it places medicines on a tiered Formulary that decides how much you’ll pay out of pocket and whether you need extra paperwork. A drug that’s "approved" for weight loss is simply listed as a covered option, often with a tier‑1 or tier‑2 designation, meaning a lower copay and less red‑tape.
Top weight‑loss medications currently on the Express Scripts formulary
Below is a snapshot of the most common FDA‑approved weight‑loss drugs that Express Scripts includes in its 2025 formulary. Availability can vary by plan, so always double‑check your specific benefit design.
| Medication | FDA‑Approved Indication | Express Scripts Tier | Typical Copay (USD) | Prior Authorization? |
|---|---|---|---|---|
| Wegovy | Chronic weight management | Tier 2 | $30‑$45 per month | Yes |
| Mounjaro | Type 2 diabetes (off‑label weight loss) | Tier 2 | $35‑$50 per month | Yes |
| Ozempic | Type 2 diabetes (off‑label weight loss) | Tier 3 | $60‑$80 per month | Yes |
| Saxenda | Obesity management | Tier 3 | $70‑$90 per month | Yes |
| Contrave | Obesity (BMI ≥ 30 or ≥ 27 with comorbidity) | Tier 2 | $25‑$40 per month | No |
| Qsymia | Obesity (BMI ≥ 30 or ≥ 27 with comorbidity) | Tier 3 | $50‑$70 per month | Yes |
| Alli | Over‑the‑counter weight loss | Not covered (OTC) | - | - |
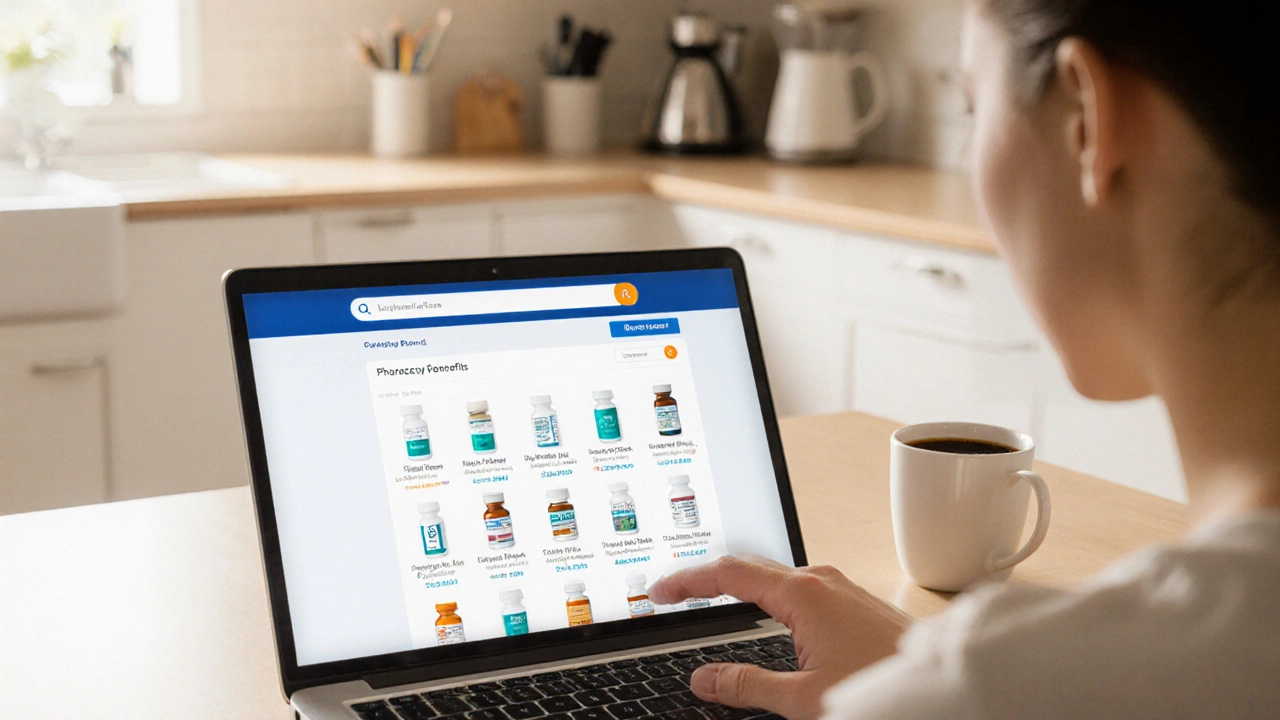
How to verify coverage for your specific plan
Even though the table above gives a good baseline, Express Scripts tailors its formulary to each employer‑ or health‑plan‑specific contract. Here’s a quick checklist to confirm if a drug is truly covered for you:
- Log into your Express Scripts member portal (or the portal your employer provides).
- Navigate to “Drug Formulary” or “Benefits Search.”
- Enter the medication name in the search bar. The result will show the tier, copay, and any restriction notes.
- If the drug shows a “Prior Authorization Required” label, be prepared to submit a short form from your doctor.
- Contact the Express Scripts pharmacy helpline (usually listed on the portal) for clarification on any gray area.

Why some popular weight‑loss drugs aren’t covered
Express Scripts balances cost, clinical evidence, and safety when placing drugs on the formulary. Drugs that don’t make the cut often fall into one of these buckets:
- Insufficient long‑term data: Newer GLP‑1 agonists may still be under review for chronic weight‑loss use.
- High price‑to‑benefit ratio: If a drug’s wholesale price is dramatically higher than alternatives with comparable results, it may be excluded.
- Safety concerns: Medications with a higher incidence of adverse events can be limited to lower tiers or excluded entirely.
- Regulatory status: Over‑the‑counter (OTC) products like Alli don’t appear on the formulary because they’re not prescription‑only.
Tips for getting a weight‑loss drug approved by Express Scripts
If your preferred medication isn’t on the formulary, you don’t have to accept defeat. Here are some practical steps that often work:
- Document medical necessity: Have your physician write a detailed note linking your BMI, comorbidities, and previous weight‑loss attempts to the need for the specific drug.
- Try a formulary alternative first: Sometimes starting with a covered option (like Contrave) can satisfy the insurer, and you can later request a switch if results are unsatisfactory.
- Leverage the “step‑therapy” exception: If the insurer requires you to try a cheaper drug first, you can request an exception stating why the step‑therapy would be ineffective for you.
- Use the patient assistance program: Many manufacturers (e.g., Novo Nordisk for Wegovy) run co‑pay cards that reduce out‑of‑pocket costs even if the drug sits on a higher tier.

Potential cost‑saving strategies
Even with formulary coverage, the price can still feel steep. Below are a few ways to keep the bill manageable:
- 90‑day supplies: Express Scripts often discounts a 90‑day fill compared to a 30‑day fill.
- Mail‑order pharmacy: Ordering through Express Scripts’ mail‑order service can shave off $10‑$15 per month.
- Manufacturer coupons: Companies frequently offer discount cards that stack with your insurance copay.
- Flexible Spending Account (FSA) or Health Savings Account (HSA): Using pre‑tax dollars reduces the effective cost.
Frequently Asked Questions
Is Wegovy covered by all Express Scripts plans?
Most commercial plans list Wegovy on Tier 2, but a few high‑deductible plans may place it on Tier 3 or require a prior authorization. Check your specific benefit design.
Can I get an OTC weight‑loss product like Alli through Express Scripts?
No. OTC products are not part of the prescription formulary, so they aren’t covered. You’d pay the retail price.
What does “Prior Authorization Required” mean for me?
Your doctor must submit a short form showing why the medication is medically necessary. Once approved, you’ll get the usual copay.
Are GLP‑1 agonists like Mounjaro and Ozempic considered “off‑label” for weight loss?
Yes. They’re FDA‑approved for type 2 diabetes, but many clinicians prescribe them off‑label for obesity. Express Scripts still covers them when a prior authorization cites the weight‑loss indication.
How long does the prior‑authorization process usually take?
Typically 2‑5 business days if the paperwork is complete. Complex cases may take a week.
Bottom line: What to do next
Start by logging into your Express Scripts account and searching the specific drug you’re interested in. If it shows up on a lower tier with a reasonable copay, you’re good to go. If it’s marked “Prior Authorization Required” or not listed at all, follow the checklist above to gather the needed documentation and submit a request.
Remember, the pharmacy benefit landscape shifts each year. Re‑checking the formulary during your plan’s renewal window (usually in October) can reveal new covered options or updated copays.
Got a favorite weight‑loss medication that isn’t on the list? Let your doctor know, request an exemption, and keep an eye on Express Scripts’ quarterly formulary updates. The right mix of clinical evidence and smart paperwork can get you the medication you need without breaking the bank.